When discussing chronic medical conditions affecting the lymphatic and circulatory systems, two distinct yet often confused disorders are lipedema and lymphedema. Lipedema vs. lymphedema: these terms are frequently interchanged, but they present vastly different symptoms, causes, and treatments.
Understanding the differences between these conditions is crucial for proper diagnosis and effective treatment. This blog aims to elucidate these differences and provide comprehensive information to aid those affected by these conditions.
What is Lipedema?

Lipedema is a chronic and progressive condition characterized by the abnormal accumulation of fat cells, primarily in the lower body. It disproportionately affects women and is often mistaken for obesity or simple weight gain. Unlike typical obesity, lipedema stubbornly resists diet and exercise interventions.
You may find an extensive discussion about lipedema here: A Comprehensive Guide to Lipedema: Types, Causes, Symptoms, Stages, Treatments, & Prevention
Causes and Risk Factors
The exact cause of lipedema is still unknown, but it’s believed to have a genetic component. Hormonal changes such as those that occur during puberty, pregnancy, or menopause may trigger the onset of lipedema.
Common Symptoms and Stages
Lipedema manifests in several stages, progressing from mild swelling to pronounced lumpy fat deposits. Symptoms include pain, tenderness, easy bruising, and swelling that does not indent when pressed—a condition known as non-pitting edema. The condition primarily affects the legs, buttocks, and sometimes the arms, while the feet and hands usually remain unaffected.
Areas of the Body Affected
Lipedema predominantly affects the legs, leading to a column-like appearance as the disease progresses. In advanced stages, the fat deposits can extend to the upper body and arms, significantly affecting mobility and quality of life.
What is Lymphedema?
Lymphedema is another chronic condition, but it involves the swelling of tissues due to the accumulation of lymphatic fluid. This blockage prevents the proper drainage of lymph, a liquid that circulates through the lymphatic system to help remove toxins, waste, and other unwanted materials.
Causes and Risk Factors
Lymphedema can be primary, occurring due to congenital defects in the lymphatic system, or secondary, caused by damage to the lymphatic vessels or nodes. Secondary lymphedema is often a result of surgery, radiation therapy, infection, or trauma.
Common Symptoms and Stages
Lymphedema progresses in stages, from mild swelling and occasional discomfort to severe swelling and irreversible skin changes. Early symptoms include a feeling of heaviness or tightness, restricted range of motion, and recurrent infections in the affected limb.
Areas of the Body Affected
Unlike lipedema, lymphedema can affect any part of the body, but it most commonly impacts the arms and legs. Secondary lymphedema often occurs after lymph node removal or damage typically visible in breast cancer patients who have undergone surgery.
Lipedema vs Lymphedema: Key Differences
While lipedema and lymphedema share superficial similarities, the differences in their underlying causes, symptoms, and treatment options are significant.
Lipedema vs Lymphedema: Differences in Causes and Development
Lipedema is primarily a genetically driven condition influenced by hormonal changes, while lymphedema results from a compromised lymphatic system, either due to congenital defects or acquired damage.
Lipedema vs Lymphedema: Distinct Symptoms and Physical Characteristics
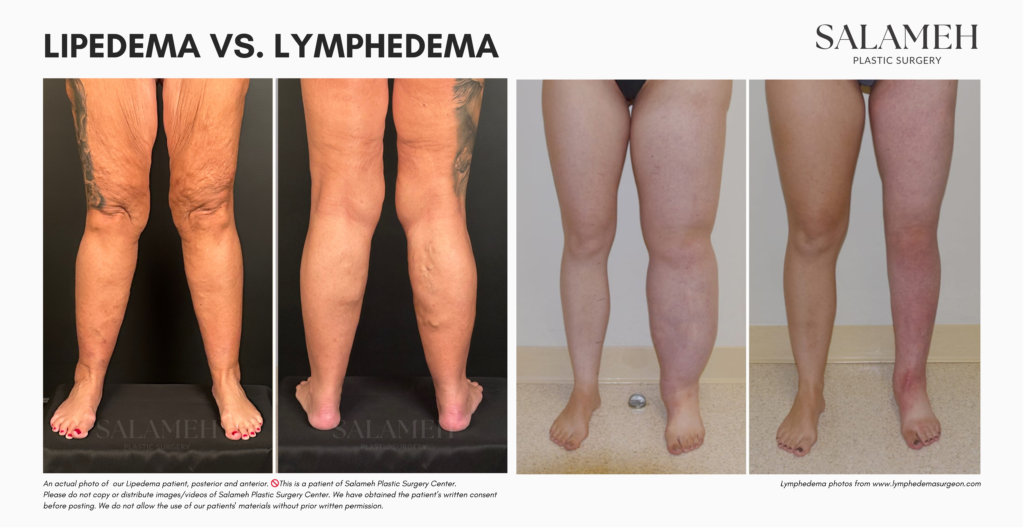
Distribution of Affected Tissues
Lipedema typically affects the lower body, sparing the feet, while lymphedema can impact any body part, often including the extremities.
Pain and Tenderness
Lipedema is characterized by pain and tenderness in the affected areas, even with mild pressure. In contrast, lymphedema usually causes discomfort due to swelling and skin stretching but is less likely to be tender to the touch.
Skin Appearance and Texture
Lipedema-affected skin remains soft and supple but appears uneven due to the lumpy fat deposits. Lymphedema can lead to thickened, fibrotic skin, particularly in later stages, resulting in a rough and hard texture.
Progression and Stages
Lipedema vs lymphedema – both progress through stages, but their trajectories differ. Lipedema stages range from subtle swelling to substantial fat deposits and deformity, while lymphedema moves from mild swelling to severe skin changes and potential disability.
Diagnosis: Lipedema vs Lymphedema
Accurate diagnosis of these conditions is crucial for effective management and requires a thorough clinical evaluation.
Diagnostic Criteria for Lipedema
Diagnosing lipedema involves a detailed patient history and physical examination. Key criteria include symmetric swelling, pain, and tenderness, predominant lower body involvement, and the presence of non-pitting edema that spares the feet. Imaging studies such as MRI or ultrasound can further differentiate lipedema from other conditions.
Diagnostic Criteria for Lymphedema
Lymphedema diagnosis also begins with a comprehensive clinical evaluation. Diagnostic tools include lymphoscintigraphy, which visualizes lymphatic flow, and bioimpedance spectroscopy, which measures extracellular fluid volume. Understanding the patient’s medical history, especially past surgeries, radiation therapy, or infections, is also critical.
Diagnostic Tests and Imaging
Both conditions may require non-invasive imaging techniques for accurate assessment. MRI, CT scans, and ultrasound can help visualize tissue composition and fluid accumulation. These tests are invaluable in differentiating between lipedema, lymphedema, and other similar conditions.
Importance of Accurate Diagnosis by Medical Professionals
Due to the overlapping symptoms and potential co-occurrence of lipedema and lymphedema, seeking evaluation from experienced healthcare professionals, such as specialists in vascular medicine or lymphatic disorders, is essential for accurate diagnosis and appropriate treatment.
Treatment Options
Management options for both lipedema and lymphedema aim to alleviate symptoms and improve quality of life.
Treatment Options for Lipedema
Conservative Treatments
Conservative treatments include compression therapy, which helps manage swelling and discomfort, and manual lymphatic drainage (MLD), a gentle massage technique that enhances lymph flow. Nutritional counseling and low-impact exercise can also support overall health.
Surgical Treatments
In advanced cases, surgical interventions like liposuction can be considered. Liposuction for lipedema is specialized to remove abnormal fat deposits and improve limb function and appearance.
Treatment Options for Lymphedema
Compression Therapy
Compression garments, wraps, and bandages are foundational treatments for lymphedema. These help maintain fluid distribution and prevent further swelling.
Manual Lymphatic Drainage
MLD is also an effective treatment for lymphedema, encouraging lymph fluid movement and reducing tissue swelling.
Specialized Physical Therapy
Complete decongestive therapy (CDT) combines MLD, compression therapy, exercise, and skincare. This multidisciplinary approach is effective in managing both primary and secondary lymphedema.
Surgical Options
In severe cases, surgical procedures such as lymphaticovenous anastomosis or vascularized lymph node transfer may be considered to restore normal lymphatic flow.
Why LippyLipo is the Best Lipedema Treatment


Living with lipedema can be challenging, but LippyLipo by Dr. Bernard Salameh, MD, FACS, offers a revolutionary solution that’s changing lives. Here’s why LippyLipo stands out as the best treatment option for lipedema:
The expertise of Dr. Bernard Salameh, MD, FACS
Dr. Bernard Salameh is a world-renowned expert in lipedema treatment.
As a double-board certified plastic surgeon and a pioneer in awake lipedema treatment, Dr. Salameh brings unparalleled expertise and a deep understanding of lipedema. His profound knowledge and dedication to advancing the field make him a trusted figure in the medical community.
Groundbreaking Awake LippyLipo Procedure
What truly sets LippyLipo apart is Dr. Salameh’s groundbreaking awake lipedema liposuction technique.
This innovative procedure utilizes local anesthesia, greatly enhancing safety and comfort for the patient by eliminating the risks associated with general anesthesia. The awake nature of the procedure allows for real-time sculpting, ensuring more precise and natural-looking outcomes.
Patient Safety and Comfort
LippyLipo prioritizes patient safety and comfort throughout the procedure.
Utilizing local anesthesia minimizes risks and ensures that patients remain comfortable and awake, allowing for immediate feedback and adjustments during the procedure.
Gentle and Precise Sculpting
Dr. Salameh’s innovative technique uses specialized microcannulas, which he personally designed, to gently remove excess fat while preserving the lymphatics. This results in precise high-definition contouring that offers both aesthetic appeal and functional benefits. The procedure’s gentle nature means reduced tissue trauma and quicker recovery.
Reduced Recovery Time
Compared to traditional liposuction methods, LippyLipo is associated with significantly shorter recovery times.
Patients can expect to return to their daily activities more swiftly without the prolonged downtime that often accompanies other surgical procedures.
Real-time Sculpting for Better Results
The ability to perform the procedure while the patient is awake allows Dr. Salameh to achieve real-time sculpting. This ensures the most accurate contouring and more satisfying, natural results, making every patient’s experience personalized and precise.
Outstanding Long-term Results
LippyLipo’s consistent, impressive long-term results make it a standout treatment for lipedema.
Patients frequently report significant improvements in pain, mobility, and overall quality of life. The results speak for themselves, showcasing life-changing transformations that restore confidence and functionality.
World-Class Care in a State-of-the-Art Facility
Salameh Plastic Surgery offers LippyLipo in state-of-the-art AAAASF-certified surgical suites. This certification represents the gold standard in office-based surgical care, ensuring that patients receive world-class care in a luxurious, safe, and comfortable environment.
Patient-centered care is at the core of Salameh Plastic Surgery’s mission, ensuring every decision prioritizes patient comfort and safety.
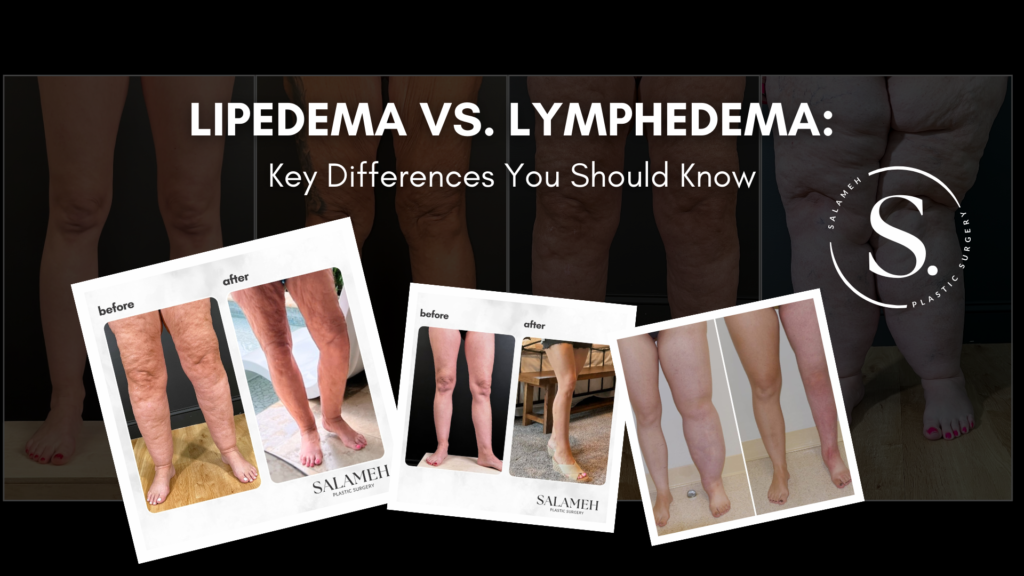
See the Transformations
Dr. Salameh combines clinical expertise, innovative techniques, and empathetic care to provide life-changing results for his patients. Explore the Before & After gallery on our website to see the transformations firsthand.
Living with Lipedema and Lymphedema
Effective management of these chronic conditions involves daily care and lifestyle adjustments.
Day-to-day Management Strategies
Implementing a daily routine of skin care, compression therapy, and gentle exercise can significantly enhance symptom control and quality of life.
Lifestyle Modifications
Adopting a balanced diet, staying hydrated, and avoiding activities that exacerbate swelling are critical lifestyle modifications. Elevating the affected limbs can also help reduce swelling.
Importance of Support and Community
Engaging with support groups and communities can provide emotional encouragement, practical advice, and a sense of connection. These networks are invaluable for those managing chronic conditions.
Psychological Impact and Coping Mechanisms
The psychological burden of lipedema and lymphedema can be substantial, leading to depression, anxiety, and body image issues. Professional counseling, support groups, and mindfulness practices can be effective coping mechanisms.
Takeaway
Lipedema vs lymphedema: although the terms might sound similar, their implications are vastly different. Recognizing and understanding these differences are crucial for effective diagnosis and treatment.
While both conditions require lifelong management, various treatments, and lifestyle modifications can significantly improve the quality of life for those affected. Raising awareness and supporting individuals with these conditions benefits not only the sufferers but also the broader healthcare community.