You’ve been working out every day for months, eating healthy, and getting enough sleep. While you can see the results in your upper body, what about the lower half? Your legs look like tree trunks. In this post, we will discuss the primary question if your current leg condition is caused by lipedema or just fat legs?
Lipedema can still occur even if you have done everything right. It causes swelling in the legs and can be painful. If you have concerns like swelling of the fat in your lower extremities, Salameh Plastic Surgery Center has the best lipedema surgeon – Dr. Bernard Salameh, who can reestablish your natural body structure and dismiss uneasiness.
Lipedema or Just Fat Legs?
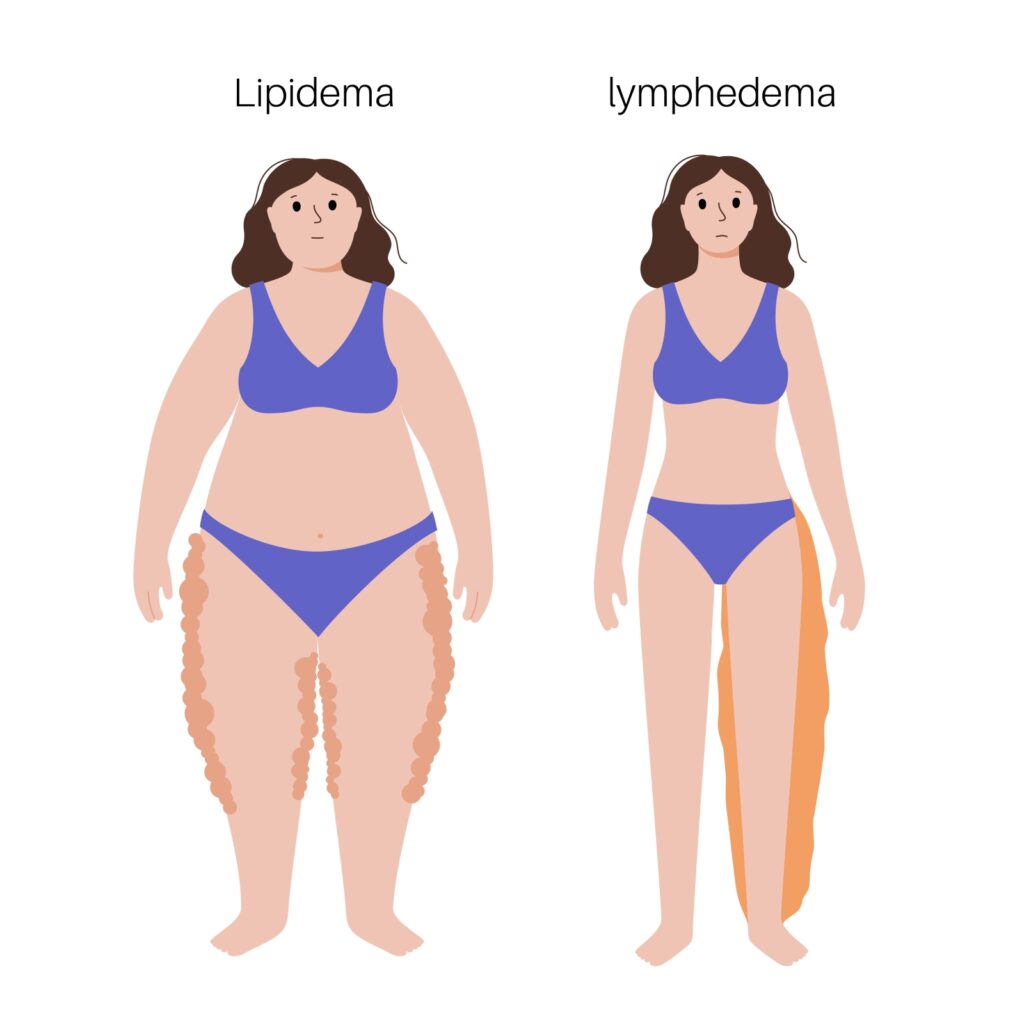
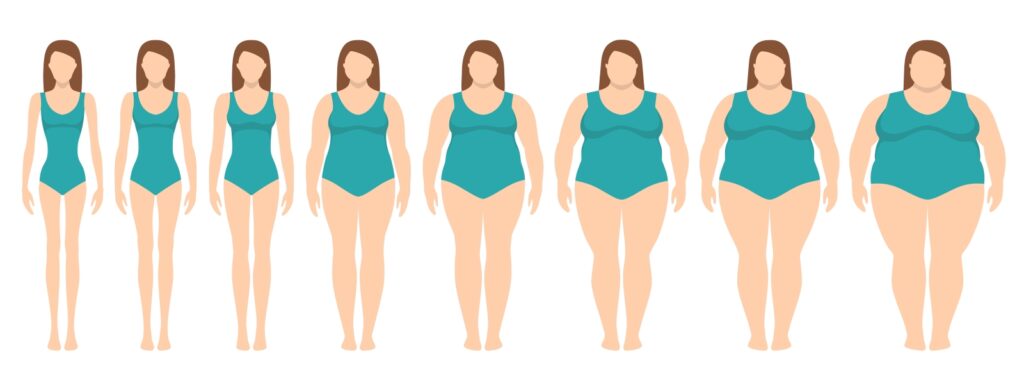
Lipedema or Lipedema Legs is a chronic condition that primarily affects women, characterized by an abnormal accumulation of fat that often results in disproportionate and painful swelling in the lower body, such as the hips, thighs, and calves.
Despite being a relatively common condition, lipedema often goes undiagnosed or misdiagnosed, leading to a significant impact on an individual’s physical and emotional well-being.
How Does Classic Lipedema Look and its Symptoms: Lipedema Legs or Just Fat Legs?
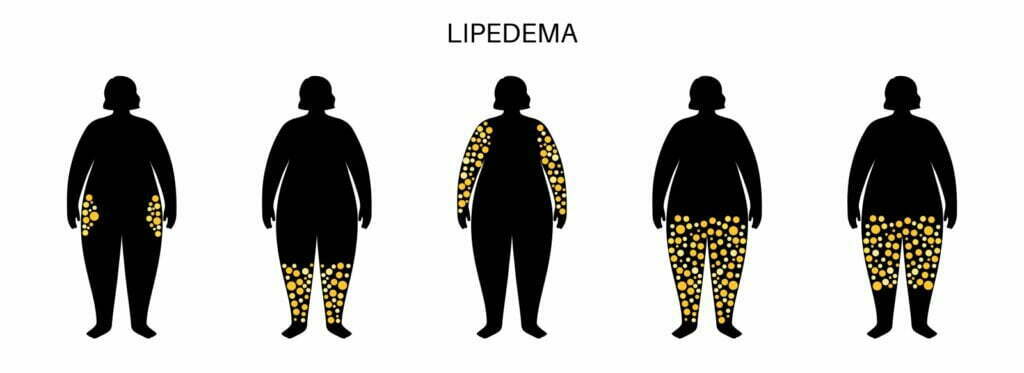
A woman with lipedema legs has a more petite upper body but a large lower body. The fat or having those fat legs is often painful. There is often more to lipedema than that. Non-classical symptoms can also be present, which appear only at certain stages of the disease progression, and other symptoms may be shared with other conditions. Let’s start by looking at the most common symptoms of lipedema.
Lipedema legs are almost always seen in women. It has been reported in men with liver disease or hormonal imbalance. The affected area is the lower body. The most common sign is excessive fat accumulation in the lower body. This usually starts at the top of your iliac crest (the bones at your waist) and continues to the lower body. Lipedema is unlikely to occur if the upper body looks obese.
Approximately 30% of patients with lipedema also experience arm edema. Typically, the upper arm is impacted in such situations. The feet and ankles are unaffected. The feet don’t accumulate as much fat as regular weight gain. However, secondary swelling can affect them. A collar of fat can often appear just above the ankles. The fat buildup could be symmetrical. Both sides of the body are impacted by fat accumulation, just like with typical weight gain. Fat accumulation can cause the legs to look lumpy or like columns. You may also notice fat deposits below your knees.
Fat legs can feel abnormal and even painful. Lipedema legs, which is a form of fat accumulation, can make fat areas feel unusually tender. Fat deposits can cause the skin to feel softer and can even cause pain.
Dr. Salameh’s LippyLipo Treatment Could the Best Solution For You

At Salameh Plastic Surgery Center, we understand the physical and emotional toll that lipedema can take on individuals. That’s why we offer awake lipedema treatments as a safe, effective, and compassionate way to alleviate the symptoms and improve your quality of life.
Our skilled double-board-certified surgeon, Dr. Salameh, utilizes advanced techniques and performs the procedures in our AAASF -Accredited state-of-the-art facilities. He is widely known as one of the best surgeon in the country who could provide the best treatment through his precise skills in targeting the abnormal fat cells that cause lipedema.
With LippyLipo Lipedema Treatment, you will remain awake and comfortable during the procedure which is under local anesthesia, allowing you to communicate with your surgeon and provide real-time feedback. Awake lipedema treatments typically result in shorter recovery periods, fewer complications, and less pain than traditional liposuction. We are committed to providing personalized care and support throughout your journey, offering practical advice on costs, scarring, and recovery.
Let us help you achieve optimal physical and emotional well-being with awake lipedema treatments at Salameh Plastic Surgery Center.
See some of our patients’ lipedema success stories here:
Pain to Power: How Leah Found Relief with Our Lipedema Treatment
Reclaiming Freedom from Lipedema: Ally’s Remarkable Journey
Other Symptoms of Lipedema/Lipoedema
Weight increase can potentially exacerbate the primary signs and symptoms of lipedema, excessive fat storage, and pain. Psychological conditions like stress and sadness can also make people more sensitive to pain and have poorer overall health.
Individuals with lipedema/lipoedema will experience increased weight gain and psychological distress if their general health and fitness are not maintained at a current level. Lipedema, contrary to popular belief, is not considered a progressive disease. This means that it shouldn’t get worse if all else remains the same. Lipedema can often worsen due to an increasing trend in obesity (which in itself is a progressive disease).
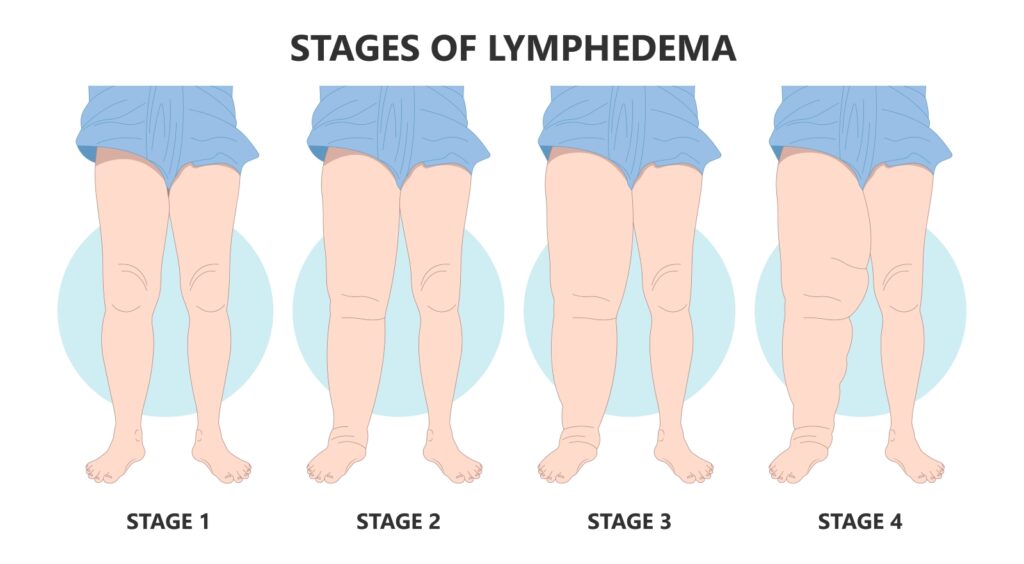
Psychological distress can also be a progressive disorder. It is characterized by increased feelings of pain, diminished willpower, and general health problems. Fluid can build up in tissues due to fat accumulation. This can cause swelling and further health problems. The so-called “lipo-lymphedema” stage appears to be the onset of what we would call obesity-induced Lymphedema. This is a condition that results from sufficient fat deposits blocking the lymph fluid’s flow out of the tissue.
Understanding the relationship between obesity, lipedema/lipoedema and lymphedema is helpful in determining which condition you are suffering from. If you’re curious about our lipedema surgery before and after, you can check our website to provide you with useful information before considering one.
How Are Fat Legs and Lymphedema Linked
Why is it that some women develop lipedema while others don’t? It appears that the disease has a strong genetic component. Lipedema is more common in women who have close relatives who have lipedema. 15% of people with lipedema have a family history. The underlying causes of lipedema are not yet known. Symptoms typically first appear around puberty. However, they can also develop after menopause or after pregnancy.
Whatever the biological cause, the initial accumulation of fat seems to trigger the development of fat deposits and pain. It is not surprising that additional fat accumulation can lead to lipedema symptoms, particularly in cases of obesity. Statistics show that body weight is closely related to lipedema. Numerous studies have shown that most patients with lipedema in Europe or North America are obese.
Even after considering the fact that lipedema patients have a high level of fat in their legs, the relationship between obesity and lipedema remains. People with classic lipedema are pretty uncommon. The size of their bottom body is greater than their upper body. This observation aligns with what we’ve seen in clinics personally.
Women are more susceptible to developing lipedema when there is a lot of fat accumulation, as lipedema can also be brought on by obesity. It appears that body weight is related to lipedema symptoms. An increase in abnormal fat and pain generally accompanies weight gain.
Lipedema patients tend to gain weight, which can exaggerate their symptoms. If left unchecked, weight gain can become progressive and eventually lead to lymphedema.
The legs, where lipedema fat deposits frequently, are also where lymphedema is more common. It is also caused by an excess of adipose tissue, which physically blocks lymphatic pathways. A person’s risk of getting lymphedema increases if they have lipedema from being overweight.
Although this common overlap might explain why the term “lipo-lymphedema” is used, we now know it to be two separate conditions: obesity and lymphedema. If you wish to undergo liposuction for personal desires like contouring or aesthetics, Salameh Plastic Surgery Center has the best surgeon and facilities to help you.
What Makes Lipedema More Difficult To Diagnose

Lipohypertrophy, which is an abnormal accumulation of fat that causes no pain, starts early in lipedema. This eventually leads to lipoedema. It can be difficult to distinguish early lipedema from weight gain in otherwise healthy people.
The likelihood of lipedema not worsening if the individual’s health and weight remain stable is high. Lipedema seems to be increasing due to the close relationship between obesity and lymphedema. This is why we need to understand the physiology and fluid transport of fat.
This is a quick explanation of fat cells and how excess fat deposits, fluid transport limitations, and lipedema can all work together to cause a worsening condition. Although the exact cause of these conditions is still unknown, some general principles can be used to explain them. Fluid transport is a crucial factor, as you’ll see.
Fat is made up of cells that need a lot of blood flow. Adipocytes are fat cells that synthesize, store, and metabolize fat. These cells don’t increase in number but grow in size with weight gain. These cells play an essential role in maintaining blood sugar balance and are fed by a lot more blood capillaries than muscle. Fluid exchange occurs in fat, so there is so much of it.
What is the Cause if the Lipedema Appears to be Progressive
Fluid balance must be maintained in fat tissue. Otherwise, swelling can occur. Fluid constantly enters fat tissue and must be removed via the lymphatic system (lymph vessels, lymph nodes) and the venous (veins, venules). These systems work together to remove the accumulated fluid. Insufficient systems can lead to swelling. Lymphedema, a chronic condition that causes swelling and is caused by lymphatic damage or congenital abnormalities, can be an example.
Patients with lipedema have abnormal fluid circulation. Hypoxic stress (low oxygen) and inflammation are believed to cause abnormal fat. Hypoxia and inflammation could result from insufficient fluid transport. One study found that the blood vessels that feed the fat deposits of people with lipedema are fragile and leaky. The small lymphatic vessels also appear to be leaky.
This suggests that patients suffering from lipedema may be more susceptible to fluid accumulation. People with lipedema have less skin elasticity. Lipedema sufferers may be more susceptible to poor fluid transportation. The skin’s elasticity creates tension that acts on the underlying tissue. This pressure helps fluid enter the lymphatic, venous, and other systems.
Studies have shown that lipedema sufferers don’t usually have visible fluid buildup, as assessed by MRI. Recent studies have shown that fluid is not usually seen in the tissue unless obesity-induced lymphedema exists. No matter if fluid circulation is affected in lipedema, it can cause disruptions in fluid transport, which in turn can lead to swelling and lymphedema.
The lower body’s fat tissue is subject to more significant pressure to maintain fluid balance and is, therefore, more susceptible to swelling. Gravity can lead to an increase in fluid accumulation in the lower body, particularly in fat tissue. This causes an increase in the demand on the lymphatic and venous systems, which drain fluid from the area.
Gravity can cause fluid accumulation in feet even in healthy people. This is why they can experience swelling from prolonged sitting or standing. The lower body’s fat tissue is more susceptible to swelling. Lipedema patients may also have abnormalities in blood vessels and a higher rate of fat accumulation. This may lead to lymphedema and swelling in their lower extremities.

Chronic swell promotes fat buildup. Swelling and inflammatory processes have been associated with fat deposition in late-stage lymphedema. Chronic excessive fluid buildup appears to promote the expansion of fat cell size and volume of tissue (nonfluid).
Although it is unclear if inflammation and blood vessel abnormalities in patients with lipedema may also be contributing to abnormal fat deposits, this hypothesis remains flawed. Lipedema doesn’t seem to progress by itself without weight gain. However, patients with lipedema at high risk for lymphedema have the incentive to stop chronic swelling.
Fat accumulation promotes even more fluid. A tissue that is larger than normal, especially fat tissue, draws more blood flow. The lymphatic drainage system has a limit on the amount of fluid it can remove from tissue. It is thought that obesity can cause secondary lymphedema. This is a condition where excess fat deposits damage and overburden the lymphatic system’s delicate vessels.
Lipedema and obesity can lead to excessive fat accumulation, which will cause fluid buildup in the lower body. If this happens, it will lead to swelling. Excess fat and swelling are common in so-called “late-stage” lipedema. This is when the patient has lipedema and obesity combined with lymphedema.
Although there is still much to be done to understand the biology of lipedema, it appears that the three are closely related. The above observations also suggest that lipedema and obesity may have a biological basis for lipo-lymphedema. Three distinct but interrelated disease processes are actually at work.
These are two reasons why compression garments are popular in ongoing lipedema management. They can be used to reduce pain and fluid accumulation (when lymphedema may be present or at risk). Research has shown that compression garments have been shown to significantly reduce inflammation and oxidative stress and improve microcirculation in both patients with venous conditions as well as healthy people.
This is a clear mechanism to reduce pain experienced by patients with lipedema who wear compression clothes. For those with lipedema who are obese enough to be at high risk for developing lymphedema, compression garments can help manage fluid swelling.
While compression garments can’t reduce fat, they can reduce pain and manage swelling in people who are susceptible or have lymphedema.
Lipo-Lymphedema and Lipedema
As we have discussed, lipedema can be seen as a progression through three conditions. These are weight gain, obesity, and lipedema. We will discuss the stages of lipedema in detail below. This coincides with how lipedema has been commonly understood and also the perceptions of many patients who have experienced the condition’s progression. We have also added the primary drivers for each stage (lipedema and obesity, as well as lymphedema).
Stage I Lipedema
This stage is when the patient has only lipedema and not obesity or lymphedema. The condition can be made worse by obesity, which will lead to more fat deposits and more pain, and mental health disorders such as stress and depression will cause more pain.
It is impossible to tell the difference between lipedema or a healthy person with more fat in their legs by just looking. In many cases, the appearance of the patient combined with other symptoms of Stage 1 lipedema may be enough to diagnose or exclude the condition. Stage 1 lymphedema should be controlled by weight management. It is not known if lipedema can lead to weight gain.
Stage I Lipedema Characteristics
The excess fat in the legs appears to be more than the fat in the upper body. Weight loss doesn’t reduce fat in this area (or even not at all). The fat is equally distributed from the hips to the ankles and affects both legs. It is possible for fat pads to appear above or below the knees making it difficult to see their normal form. There is also no excess fat or swelling at the feet or ankles.
The skin can also appear healthy and not discolored. Pressure can also make fat painful. Lipedema can make fat deposits feel painful when pressure is applied. This is unlike women who are healthy with slimmer legs and women with lymphedema. Although they are not under any strain, some people may experience the pain of fat deposits on their own. Any over-the-counter medicine is typically ineffective for treating this kind of discomfort.
Fat is not normal. Lipedema can lead to fat deposits that are more susceptible to bruising. This is due to the tissue’s microvascular fragility (blue spots may appear after minor events) as well as inflammatory markers in the fat tissue. It may be squishy, but it may not have the same consistency as other upper body fat. Fat nodules that are small and homogenous may also be present.
Stemmer’s sign is negative. You can pinch and lift the skin at the top of your foot, near the toes. Stemmer’s positive sign means that the flesh at the top of each toe feels firm and can’t be pulled or pinched. This test is used to determine if there is any swelling or fibrotic tissue on the feet. Stemmer’s sign indicates positive when lymphedema affects the feet.
When thumb or finger pressure is applied to the fat area, there is no “pitting”. Another indicator of swelling is thumb pressure. Another indication that swelling is fluid-related rather than the result of fat accumulation is this. In Stage 1 lipedema, there may be brief ankle or foot swelling toward the end, but it will go away with elevation or sleep.
Stage II Lipedema
This stage is when the patient has lipedema and a pronounced body weight gain/obesity. There is no lymphedema. As in Stage 1, the patient’s condition deteriorates. Stage 1 lipedema frequently advances to Stage 2 in the absence of good weight management. Lipedema is driven by weight gain and obesity, which tend to be progressive.
The affected areas may begin to acquire larger lumps of fat. Fatty nodes may be felt quite easily. Small fatty nodules, which are not smooth but can be felt in the tissue, can be felt easily. Skin can appear uneven and textured, as well as discolored.
Stage III Lipedema (also known as lipo-lymphedema)
This stage is when the patient has obesity-induced lipedema and lipedema. The patient’s condition worsens as a result of mental health disorders such as stress, depression, and anxiety (which can lead to more pain). Lipedema can develop over time. On average, it takes 17 years.
Stage III Lipedema Characteristics
There is lymphedema swelling. Stemmer’s sign could be positive. The backs of the feet and ankles are swelling, which may indicate that fluid has formed from secondary lymphatic insufficiency. Chronic lymphedema is a condition where the swelling doesn’t disappear after one night of sleep. This lymphedema can become chronic if it isn’t treated.
Thickened, hardened skin that shows some discoloration. Advanced cases of lipedema, where lymphedema is also present, can cause tissue hardening. Long-term edema, fibrosis, a lack of skin suppleness, and fat deposition can all contribute to this. Legs are no longer symmetrical. On the legs, asymmetrical fat masses, fibrotic tissue, and swelling might grow. This may make it difficult for the leg to move normally.
How Can Lipedema Be Commonly Diagnosed?
It is not common and not often. Although it has been reported that 11% of women are affected by lipedema, our knowledge and appreciation of the disease are still limited. We don’t know the exact prevalence of lipedema. Published estimates range from 1 in 72,000 to 1 per 5 women.
Lipedema is a relatively new condition. It is sometimes mistakenly diagnosed as either obesity (a common form of lipedema) or primary lymphedema (a congenital type of lymphedema that can affect both sides of the body). Lipedema is not easily diagnosed because there aren’t any standard protocols or tests.
Obesity, lipedema, and lipo-lymphedema (lipedema and simultaneous lymphedema) are best diagnosed through a physical examination with palpation, combined with an examination of the patient’s clinical history, and not by diagnostic tests. Because lipedema can have a hereditary component, it is possible to use family history.
Should I Self-Diagnose or Contact a Doctor?

Consult a doctor immediately if you experience unexplained swelling. There are many possible causes of unexplained swelling. Some can be very serious. Talk to your doctor if you have any concerns about swelling in your legs or elsewhere. It can be challenging for people suffering from lipedema to receive a timely and accurate diagnosis. It is not an easy test, so it takes some detective work to diagnose lipedema.
You can self-diagnose this condition if you suspect it. Lipedema is a common condition that many family doctors don’t know much about. Your self-investigation could help you get a formal diagnosis. Although a self-diagnosis can’t replace a professional diagnosis, it can help you to direct your care and obtain the diagnosis you want. Seek some qualified health professional who is knowledgeable about lipedema, it may be worth speaking with them.
This is how to self-diagnose lipedema or lipo-lymphedema and also how to effectively seek a formal diagnosis. Check to see if there is a family history, and you should be familiar with the stages of lipedema, the conditions of obesity and lymphedema that are related to it, and the symptoms.
Write down your symptoms. What symptoms are you experiencing right now? You may feel a difference in the fat texture in your affected areas and other body parts. Are they different? Are your symptoms consistent with the above stages of lipedema? It can be difficult to assess your own body objectively, even for professionals in health. Is there pain in your fatty tissue?
What has changed in your symptoms over the years? Are you a victim of weight gain that has led to leg symptoms getting worse? Draw a timeline of your symptoms. When did you notice anything developing? How did your symptoms change over time? Are there any other symptoms you experience that are not listed above? Administer a record to keep a check of any additional symptoms.
The above steps may help you to rule out or at least reduce the likelihood of you having lipedema. Numerous other ailments may cause comparable symptoms. This is why it is essential to discuss your findings with your family physician. Talk to your doctor about your symptoms and your family history, and let them know you think you may have lipedema. Your physician may not have the best knowledge or experience with lipedema.
They may think your symptoms are due to lipedema, but they might be wrong. You should also be open to the possibility of lipedema not being present and that your symptoms could be due to another condition. Your doctor may be unable to explain your symptoms, or they don’t have enough knowledge about lipedema. You can ask for a referral. A vascular surgeon, dermatologist, plastic surgeon, or physician who treats obesity-related diseases may all have some knowledge about lipedema.
How Can Lipedema Be Treated?

A diagnosis is essential for the proper treatment of lipedema. Lipedema is not something that many healthcare providers are familiar with. You may be able to see a specialist if you suspect that you might have lipedema. Vascular specialists are usually well-informed about common causes of leg pain and can help you rule out other contributing factors. Lipedema is usually treated with:
Compression
Compression clothes can be used to push inflammatory products from the legs and stop them from building up. It should be worn throughout the day and taken off at night before bed. Regular use of compression garments that fit well can reduce swelling and remodeling of the affected limbs. Patients with lipedema may find compression garments uncomfortable. There is some trial and error.
There are also many options like knee-high socks, thigh-high stockings, and pantyhose. Because there is no tight band around the legs, compression leggings can be more comfortable.
If there is swelling around the feet, you should avoid wearing leggings. Start with a lighter compression (15-20mmHg) and then work your way up to a tighter compression (20-30mmHg).
A pneumatic compression pump, which is a device that compresses air through sleeves on the legs, may be beneficial for some patients. It allows the patient to massage the legs gently and encourages the flow of lymphatic fluid.
Diet
Anti-inflammatory diets may be beneficial for patients with lipedema. Avoid pre-made and processed foods and instead opt for whole-food or homemade options. Avoid meat and saturated fats, and opt instead for a plant-based diet that occasionally includes lean proteins. Get more fruits and vegetables and plenty of water.
You can add natural anti-inflammatory agents like turmeric and garlic to your cooking, or you can use a supplement. To slow down the progression of the disease, weight management is essential. A higher chance of symptoms developing or worsening is associated with more fat. It is important to note that weight loss is not a treatment for lipedema.
Exercise
Regular, low-impact exercise can be used to force the inflammatory products out of the tissues. The effects of hormonal fluctuations can also be reduced by exercising. Swimming, cycling, and walking are all good options for lymphatic drainage. They also improve blood flow to the affected limbs. High-impact exercise (i.e. Avoid contact sports, such as jogging or step-aerobics). They can cause joint pain and bruises.
It is especially beneficial to exercise in water. It helps to relieve pain and improves lymphatic and vein function. It provides gentle, gradual compression to the legs and is safe.
Liposuction
Patients can become discouraged if weight loss does not alleviate their pain. They may not notice a difference in the length of their legs. For better results, liposuction may be an option for patients with lipedema. Many patients find that liposuction is very effective in removing fat cells. Unfortunately, insurance coverage is not available for this procedure. Make sure you consult a liposuction specialist in treating lipedema.
Liposuction is the most common surgical procedure for lipedema. The most common liposuction techniques for lipedema include water-assisted and tumescent anesthesia liposuction. Tumescent liposuction uses tumescent to infuse the subcutaneous tissues with tumescent to cause fat cells to swell. Vessels then constrict, and micro-cannulas are used for suction.
At Salameh Plastic Surgery Center, we offer awake lipedema treatments as a safe, effective, and compassionate way to alleviate symptoms and improve your quality of life. Our world-renowned surgeons utilize advanced techniques in targeting abnormal fat cells. Awake lipedema treatments result in shorter recovery, fewer complications, and less pain than traditional liposuction. Let us help you achieve optimal physical and emotional well-being with awake lipedema treatments at Salameh Plastic Surgery Center.
Vascular Care
Patients with lipedema might also have deep- or superficial vein disease, which could be contributing to their symptoms. While vein disease can be difficult to spot, there are some symptoms that may indicate it.
Varicose and spider veins and leg swelling are examples of vein disease symptoms. Leg discoloration or darkening around the ankles or calves of the skin is also one. Fatigue or weight loss in the legs can also indicate that you have a vein disease around your legs. Leg itchiness or restlessness and some leg symptoms, such as swelling and discomfort, can be relieved by treating vein disease.
Lipedema Plastic Surgeon in Indiana & Kentucky

Are you seeking effective treatment for Lipedema without the use of general anesthesia? Salameh Plastic Surgery Center is your destination. Our skilled plastic surgeons are pioneers in Awake Lipedema Treatment, offering a comprehensive approach to address this often misunderstood and underdiagnosed condition.
With our Awake Lipedema Treatment, you can experience less pain and downtime while still achieving exceptional results. By avoiding general anesthesia, the risks associated with it are minimized, ensuring your safety throughout the procedure. Our surgeons utilize advanced techniques and state-of-the-art equipment to target and remove excess fat in affected areas precisely, improving your body shape and reducing discomfort.
Schedule Your FREE Consultation Today!
At Salameh Plastic Surgery Center, we pride ourselves on providing personalized care and support to each patient. Our experienced and compassionate staff will guide you through every step of the process, from consultation to recovery. By choosing our clinic, you are taking a proactive step towards improving your quality of life and achieving your desired body.
Discover the advantages of Awake Lipedema Treatment at Salameh Plastic Surgery Center. Contact us today to schedule your consultation and embark on a transformative journey toward a more comfortable and confident you. Let us help you regain control over your life.
If you want additional information about them, you can visit us on our Meet Our Surgeons page and check their expertise, experience, and achievements.
A consultation with one of our plastic surgeons in Indiana or plastic surgeons in Kentucky should be arranged to estimate your needs for the lipedema surgery. The procedure is performed in Salameh Plastic Surgery Center – AAAASF-certified surgical facilities, which will make sure you are safe and convenient during and after the procedure.
Takeaway
Lipedema is a serious condition that can cause severe impairments in the quality of the patient’s life. While lipedema is a chronic condition, it can be managed as many other chronic conditions. Many patients suffering from lipedema experience significant improvements in their symptoms and can live well long-term with proper treatment.